The first 1,000 days of life, from pregnancy to second birthday of the infant, are extremely critical since poor nutrition and recurring bouts of infection may result in the often-irreversible consequence of stunting, followed by short adult stature. Previous research indicates that adult height can be a marker of health. Even after accounting for factors like education and income level, the association between short stature and adverse health outcomes remains. Further evidence illustrates that shorter maternal height leads to poor obstetric, neonatal and fetal outcomes such as a higher rate of unnecessary cesarean section (c-section), under-five mortality particularly in the neonatal phase, preterm birth and stillbirth among other conditions.
A paper recently published in PLOS ONE by Arendt et al. examines the association between maternal height and c-section as well as maternal height and neonatal mortality in 34 sub-Saharan African countries, a region facing numerous maternal and neonatal health challenges along with the smallest gains—even losses—in average adult height during the last century. The authors used the most recent Demographic and Health Survey (DHS) data to study the heights of women (20 years or older) who had given birth in the last five years since the survey. This study is the first of its kind to apply categorical height cut-offs—from very short to tall—in looking at the effect of maternal height on c-section rates as well as neonatal mortality by age at death.
Maternal height and c-section rates
In analyzing data from 34 countries, authors were able to adjust for multiple socio-economic factors given that c-section rates are likely to be higher among more educated, wealthier and urban women. Research findings indicate that short maternal height is associated with increased rates of c-section, even after controlling for income, education and residence. The study also found that c-section rates were related to having a previous cesarean section.
The higher rates of c-section accompanied by meager gains in height during the past years warrants attention due to challenges in access to c-section infrastructure in the sub-Saharan region. C-section rates for the countries analyzed in the study are widely below the World Health Organization benchmark. Such low rates, at below 10%, indicate that economically disadvantaged women often cannot access medically-indicated, lifesaving c-sections.
Maternal height and neonatal mortality
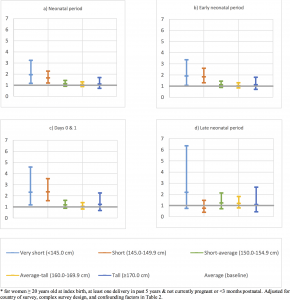
The study results illustrate that shorter women undergo more neonatal losses as compared to average height women. These findings resonate with other studies exploring similar relationships. Further, as the paper is novel in its approach to define neonatal mortality by age at death specifically, its findings also demonstrate that the effect of maternal stature was stronger on the infant’s first days of life – day 0 and 1.
A higher number of deaths on first day of birth points towards the challenge of birth asphyxia faced by infants born to very short and short women. This interpretation is also supported by study results expanding on the relationship between maternal height and c-section rates since c-sections are often associated with complicated or prolonged labor. Additionally, babies born to shorter women via c-section are least likely to experience skin-to-skin contact and breastfeeding in the first hour of life which are protective practices for newborns. Furthermore, research shows that short maternal height is linked to higher rates of stillbirth. Unfortunately, DHS does not report data on stillbirths and hence this study does not include stillbirths in its analysis.
Why does it matter? Cost to individuals and the system
Short stature of women is related to increased c-sections and infant mortality. Higher rate of c- sections in the context of health infrastructure barriers in the sub-Saharan region can cause high cost to the families as well as to health care systems. C-sections can be lifesaving in critical situations, but, when not medically indicated, they can pose financial challenges as well as health complications for mother and child.
Policy implications
The research findings of the paper serve to argue for policies targeting stunting among infant girls, extending through adolescence for potential catch-up to increase adult height. Even though it was assumed that adult stature is mostly dependent on averting stunting during the first two years of an infant’s life (first 1,000 days), recent studies have indicated that some catch-up might take place in early childhood. Policies for reducing stunting in infant girls, aiming to increase their adult height and thereby potentially reduce the risk of adverse birth outcomes later in childbearing years, must be strongly advocated.
—
Read the full paper, “Effect of maternal height on caesarean section and neonatal mortality rates in sub-Saharan Africa: An analysis of 34 national datasets,” in the MHTF-PLOS collection on noncommunicable diseases and maternal health.
Explore other posts from the Maternal Health Task Force’s blog series, “Noncommunicable Diseases and Maternal Health.”
