Background: Afghanistan has one of the highest infant mortality rates in the world with estimations between 52 and 110 per 1,000 live births in 2017, depending on the source.[1],[2] In addition, thousands of Afghan women die each year from preventable pregnancy-related causes; 396 maternal deaths per 100,000 births.[3] These figures are alarming enough, however many agencies assert that the actual figures are in fact much higher and that the actual maternal mortality ratio is likely to lie between 800 and 1200 per 100,000 live births.[4] The situation is particularly bad in rural and difficult to reach areas, where as few as 3% of deliveries are attended by a skilled professional.[5]

Table 1: Maternal and Newborn mortality in Afghanistan, 2002-2015
| Mortality Rate | Year | |||
| 2002 | 2005 | 2010 | 2015 | |
| Maternal mortality rate (MMR) (death per 100,000 live birth) | 1600 | 821 | 584 | 396 |
| Newborn Mortality rate (death per 1000 live birth) | 165 | 129 | 77 | 45 |
Other estimates show the risks are even worse: a 2015 survey indicated 1 in 14 women in Afghanistan die of pregnancy-related causes.
The 2014 report from United Nations Population Fund (UNFPA), in partnership with the World Health Organization (WHO) and the International Confederation of Midwives (ICM) ‘The State of Afghanistan’s Midwifery 2014’ states that only 23 percent of the needs for maternal and reproductive health services in Afghanistan are currently being met.
Afghanistan has an enormous need for qualified midwives. The country has only 3.2 nurses or midwives per 10,000 people, according to the World Health Organization.
Under Taliban rule (1996-2001) women were banned from working and studying, leading to an acute shortage of midwives. On-going conflict, internal displacement and difficulties in women accessing education and employment have added to the shortage of midwives in Afghanistan. The government has sought to address this issue by reducing the training period from 4 years to 18 months in the Community Midwifery Education Program. Although this policy has led to an increase in the overall number of midwives, the breadth and depth of their skills and knowledge has been compromised.
It is difficult to give an exact number of midwives available in Afghanistan as no live registry of licensed midwives exist. The following table is based on data from the Afghan government.
Table 2. Midwife availability in Afghanistan 2002-2017
| Year | 2002 | 2008 | 2014 | 2015 | 2016 | 2017 | |
| Number of Midwives | 467 | 2,167 | 4,600 | 3,426* | 2,349* | 3,302* |
* The numbers corresponding to 2015, 2016 and 2017 may not reflect the engagement of community midwives, who are not certified by the Ministry of Public Health but are trained and contribute to the success of the maternal and neonatal wellbeing around the country.
Skills-Gap Training:
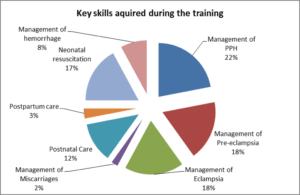
Action for Development (AfD) has developed a training program aimed at directly addressing these skills gaps. Through partnership with the Geneva Health School, University of Applied Sciences Western Switzerland (HEdS) training modules were developed in 5 key areas; eclampsia, pre-eclampsia, management of the third stage of labour, post-partum haemorrhage and care of the newborn.

The overall objective of the training is to reduce maternal and infant mortality rates in rural areas of Afghanistan through improvement of the skills and competences of the midwives.
Specific objectives are:
- Increase the proportion of pregnant women who receive ante-natal care
- Increase the proportion of births attended by qualified midwives
- Expand the use of family planning services
- Improve the management and treatment of the most common complications during pregnancy and birth
- Increase the demand for care through community outreach.
Focusing on midwives in rural Afghanistan, AfD has trained 490 midwives since 2014 in 7 provinces – Kapisa, Herat, Parwan, Bamyan, Panjsher, Takhar and Kabul. After receiving the training, each midwife is able to go on to train an average of 5 other midwives in a cascade model of training, supervised by the Ministry of Public Health (MoPH).
In 2017 AfD undertook an evaluation of the program to assess its impact. The full findings are available in this report.[6]
Summary of Findings:
Analysis shows that 100% of midwives participating in the training affirm that it has allowed them to better handle pregnancy, deliveries, newborn care and related complications. In addition, the midwives interviewed said that the training filled gaps in their knowledge and increased their professional confidence.
The evaluation also shows that there was an increase in the satisfaction rate of communities receiving services from the midwives. Furthermore, HMIS (Health Management Information System of the MoPH, Afghanistan) data depicts an increase in pregnant women receiving antenatal and postnatal services at the health facilities by 19% and 30% respectively in the period 2013-2016.
Additional data covering the three-year training period in all five provinces indicates:
- 12% increase in the number of pregnancy related consultations
- 10% increase in the number of deliveries in health facilities
- 26.5% increase in the number of family planning consultation
Ministry of Public Health Officials who participated in the evaluation had the following observations.
Benefits of the program included:
- increased knowledge and capacity of the midwives
- increased interaction between midwives, which has facilitated an increase in the sharing of knowledge and experience
- improvement in the trust local people have in their community healthcare providers
- improvement in the prevention of complications during pregnancy and childbirth
- reduction in infant mortality
- reduction in maternal mortality
And the following recommendations:
- increase the duration and frequency of the training
- expand the number of topics covered by the training
- roll out the training to more provinces
- increase the number of partners in order to increase funding
Factors to Consider Going Forward
The evaluation revealed three potential risk factors to the future success of the project:
1) Under-investment in healthcare means that in some cases health centres lacked the necessary equipment and medication, infrastructure and staff capacity for the trainers to carry out the training in the best possible way.
2) A shortage of midwives generally means that those who are practising have a heavy workload and sometimes not enough time to cover subjects beyond immediate care e.g. family planning advice.
3) An increase in budget will be needed to roll out the recommended improvements.
2019 is an exciting year for AfD’s midwife training project. A new nutrition module is planned for completion by the end of the year. We are collaborating with the MoPH to include the new Maternal Child Health Handbook in our programme and finally, through continued partnership with HEdS, Switzerland and funding from the Conservation, Food and Health Foundation, Boston, Massachusetts, five new training modules have been produced[7] and will be rolled out across additional provinces in 2019, 2020 and beyond.
References
[1] http://www.childmortality.org/files_v22/download/UN%20IGME%20Child%20Mortality%20Report%202018.pdf
[2] https://www.statista.com/statistics/264714/countries-with-the-highest-infant-mortality-rate/
[3] WHO, Afghanistan: country profiles; Maternal mortality in 1990-2015
[4] https://www.theguardian.com/global-development/2017/jan/30/maternal-death-rates-in-afghanistan-may-be-worse-than-previously-thought
[5] https://www.sciencedirect.com/science/article/pii/S2214109X17301390
[6] http://www.actfordev.org/presentation/documents/
[7] Obstructed Labour, Family Planning, Infections, Miscarriage Care and Manual Vacuum Extraction
